Acute or chronic?
Editor's note: Kathleen Evans is senior vice president at research and consulting firm Healogix. Catie Barbieri is director at Healogix. Stacey Cowgill is senior director at Healogix.
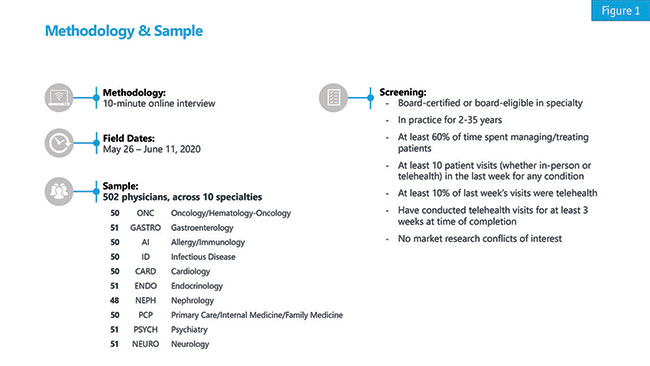
COVID-19 has changed the way people all over the world work and live and physicians are certainly no exception. To understand the impact of COVID-19 on physicians in the U.S., Healogix fielded a quantitative survey in spring 2020. We reached 502 physicians across 10 specialties to gain their perspective on this unprecedented time and how it may be affecting their practices. For more detail on the sample included and the screening criteria, please see Figure 1.
Use of telehealth
Prior to COVID-19, 68% of physicians surveyed did not use any form of telehealth in an average week. When asked why, about half cited reasons such as less favorable insurance coverage/access, less favorable reimbursement and the perception that it is a less effective way of practicing medicine compared to in-person visits. Of those surveyed who did not regularly conduct telehealth visits before COVID-19 restrictions, 42% indicated they did not have the capability, with this percentage being particularly higher for physicians in hospital-based practices (56%) than in community-based practices (35%). In a separate line of questioning, hospital-based physicians were also significantly less likely to agree that nearly all their patients have access to the technology necessary to conduct telehealth visits either, as compared to community-based physicians.
In terms of physician specialty, psychiatrists appear to be the most telehealth-friendly specialty as they were more likely to be already utilizing telehealth before COVID-19 restrictions were implemented and reported the highest volume of telehealth visits since the restrictions began (84%). Prior to the pandemic, the vast majority of gastroenterologists (80%) and allergists/immunologists (84%) reported not conducting telehealth visits in an average week. However, gastroenterologists reported the second-highest volume of telehealth visits since restrictions were implemented (69%), while allergists/immunologists were significantly lower, at 49% of their visits. Oncologists reported the lowest volume of patient visits as telehealth since restrictions were implemented, at 45%.
How physicians engage in telehealth visits has also changed since the pandemic began. Prior to COVID-19, physicians were using phone calls with no video component most often. However, during COVID-19 the use of video-enabled calls such as Zoom or FaceTime rose significantly and replaced phone-only calls, except among Midwest physicians, who reported using phone-only calls significantly more often than their counterparts in the West and South (35% of visits versus 27% and 23%, respectively). Use of telehealth-enabling apps such as Doximity, Doxy.Me or Teladoc and EMR systems such as Epic or Cerner did not change significantly due to the pandemic. At the time of the survey, most physicians reported using two or more of these modalities to conduct their telehealth visits.
About half of physicians included in the survey reported that both they and their patients are satisfied with telehealth visits, while about one-quarter feel neither party is satisfied. Physicians with a higher volume of younger patients (i.e., <55 years of age) tend to feel both parties are satisfied more than their counterparts with an older patient base (55% vs. 41%, respectively). While most physicians did report feeling satisfied, there were some concerns. About two-thirds worried about missing clinically important cues via telehealth and nearly half had concerns about the quality of care they are able to provide via telehealth and their ability to record all necessary clinical measurements for their specialty and patients in a telehealth visit.
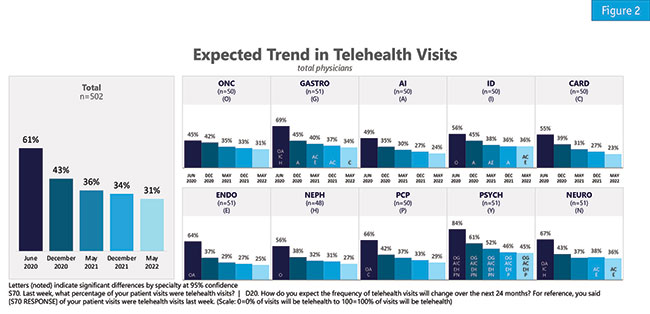
Looking to the future, physicians expect the proportion of telehealth visits to decline as they move through 2021, though they do expect about one-third of their visits to still be via telehealth by early 2022 (Figure 2). Consistent with use of telehealth pre-COVID restrictions, psychiatrists anticipate conducting a significantly higher volume of telehealth visits through 2021 and into 2022 than other specialties surveyed. One in five physicians overall and 39% of psychiatrists – a significantly higher proportion that all other specialties surveyed – expect the majority of their patient visits will be telehealth in May 2022 for reasons such as convenience, COVID-19 uncertainty and a belief that telehealth is the future of health care. Only 10% of allergists/immunologists surveyed believe the majority of their patient visits will be telehealth in May 2022. After COVID-19 restrictions have eased, physicians overall expect about two-thirds of their patients will feel comfortable enough to return to the office in person.
While telehealth is unlikely to constitute the majority of visits for most physicians surveyed if/when COVID-19 restrictions ease, telehealth does appear to be here to stay in a more significant way than pre-COVID-19. Given the perception of telehealth as a less effective way to practice medicine by many physicians surveyed, this presents an opportunity to support physicians as they make a transition to more regularly scheduled telehealth visits. When asked how a pharmaceutical manufacturer could support their use of telehealth, most ranked PDFs/electronic handouts for patients as most preferred, followed by websites for patients and then webinars for patients. Unaided, 35% indicated patient education materials would be helpful and 24% want better access to samples and copay cards for patients they see via telehealth. By providing these materials to assist physicians in helping their patients, pharmaceutical companies can improve physicians’ comfort with telehealth moving forward.
Easily accessible and straightforward platforms will also likely provide needed support to physicians and patients as they move forward with telehealth. With the drop in preference for phone-only calls, video-enabled platforms will likely be preferred among physicians across the board for telehealth visits. Also, given the perception by many physicians that they or their patients do not have access to the necessary technology, education on the types of platforms/apps available and ensuring easy access will be crucial for future telehealth visits for physicians and patients alike.
Clinical activities
At the time of surveying, physicians of all specialties reported experiencing a significant drop in weekly patient volumes, with an average decrease of 28% and primary care physicians (PCPs) and gastroenterologists being most notably affected with 38% and 41% decreases, respectively. When it comes to comparing clinical activities via telehealth during COVID-19 vs. in-person before COVID-19, physicians indicated they were switching and/or initiating treatment about one-third less often. Of note, oncologists reported initiating treatments about half as often. Orders for routine lab work appear to be the least affected by COVID-19. 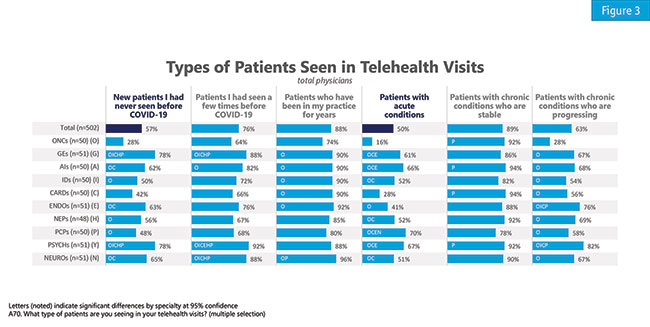
Physicians also reported seeing new patients about half as often as before COVID-19 restrictions were implemented in their current telehealth visits, with PCPs and allergists/immunologists reporting their new patient volume is 38% and 39%, respectively, of what it was prior to pandemic restrictions. When asked what type of patients physicians are seeing (Figure 3), only 28% of oncologists reported seeing new patients at all via telehealth, which is significantly lower than every other specialty surveyed except cardiologists. Additionally, fewer physicians overall reported seeing patients with acute conditions via telehealth than other patient types in telehealth visits. The vast majority of physicians indicated they are using telehealth to see patients who have been in their practice for years (88%) and patients with chronic conditions who are stable (89%).
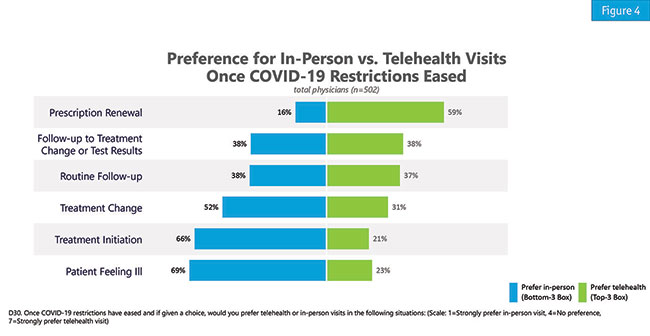
In the future, the majority of physicians surveyed would prefer to see a patient in person for things like illness, a treatment change or treatment initiation and handle prescription renewals via telehealth (Figure 4). Those living in areas with higher volumes of COVID-19 cases have an even stronger preference for the use of telehealth for prescription renewals. Unsurprisingly, physicians who didn’t begin using telehealth regularly until after COVID-19 restrictions were implemented would prefer to go back to in-person visits at a higher rate across all situations.
Switching and initiating treatments via telehealth are areas with potential for significant implications for pharmaceutical companies moving forward. Ensuring access to samples for patients seen via telehealth could regain some of the switching activity that has been lost due to COVID-19. This may be an area of interest for physicians when they connect with sales reps and reps should be prepared to discuss how they can help. Support for co-pay card enrollment with electronic materials for patients and physicians’ practices may also be an important element in ensuring patients can switch or be initiated on a medication, particularly when many patients are likely experiencing employment or other financial uncertainties.
Reductions in clinical activities may also be a direct consequence of reduced patient volumes, particularly for seeing new patients. Supporting use of telehealth both on the physician and patient side may prove beneficial in regaining lost patient volume as both physicians and patients become more comfortable with the modalities. While many physicians would prefer to return to in-person visits once pandemic restrictions permanently ease and believe most of their patients will feel comfortable enough to return in-person to the office when they do, it is difficult to predict when this will happen. It is worth further investigation to see how these physicians’ views on telehealth for specific clinical activities change as they become more accustomed to telehealth visits with their patients and what resources they feel they need once they become more comfortable using telehealth. Also meriting more investigation is how patients feel about transitioning to telehealth, the types of visits they would be comfortable making appointments for via telehealth moving forward and when they expect they will feel comfortable enough to return to physicians’ offices in person.
Sales rep interactions
Looking to sales rep interactions, reps have been connecting with physicians most often through e-mail, followed by phone calls and video-enabled calls. However, at the time of the survey, about one-quarter had not interacted with a sales rep at all since COVID-19 restrictions began. This figure was higher among PCPs (30%) and infectious disease specialists (IDs) (34%) and lowest among endocrinologists (12%) and neurologists (16%). Physicians age 56+ (26%) were also significantly less likely to have interacted with a rep than physicians age 26-40 (13%).
A transition to remote rep visits brought on by COVID-19 is not an issue for most who participated in the survey. When asked about their preference for remote versus in-person, the majority either preferred remote or had no preference while about one-third preferred in-person interactions. Physicians who were regularly conducting telehealth visits prior to COVID-19 restrictions were significantly more satisfied with remote sales rep interactions than their counterparts and were significantly more likely to prefer scheduling a remote appointment. This suggests a generally higher comfort with remote-based communications in general.
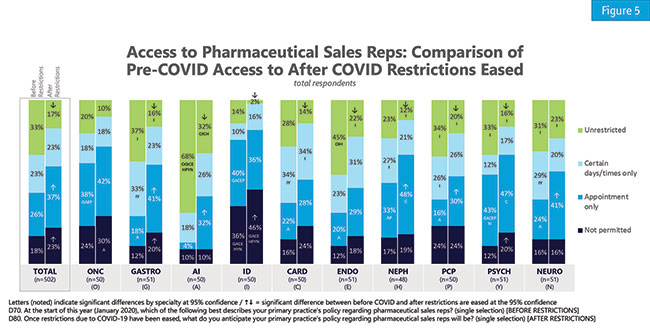
When asked about anticipated changes to sales rep policies, the majority believe rep access will not permanently change due to COVID-19. For those who do foresee a change, most anticipate more restrictions, from reps needing to make appointments to them having no access at all to their practice (Figure 5). IDs report a policy of “not permitted” most often, both before COVID-19 restrictions were put in place and when anticipating a post-COVID scenario. Gastroenterologists and psychiatrists also anticipate significant increases in “not permitted” policies once COVID-19 restrictions are lifted. Allergists/immunologists foresee the largest drop in “unrestricted” access, going from 68% pre-COVID to 32% after COVID-19 restrictions are lifted.
Pharmaceutical and biotech companies will need to devise new, engaging strategies to connect with these practices that restrict their access. While most physicians do not anticipate permanent changes to their practice’s rep policies once restrictions have lifted, it is unclear when or if in-person restrictions will ever be completely rescinded. Virtual detailing is likely to play an important role moving forward. It is a good sign that most physicians are reasonably satisfied with remote rep interactions early on in their implementation and as physicians become more comfortable with virtual appointments in general – including telehealth – satisfaction and comfort with these rep encounters will likely rise as well.
As with telehealth, there is also an opportunity to develop innovative apps for seamless communication using electronic detail aids with sales reps and medical science liaisons as they continue to engage in virtual detailing. While not assessed in this study, it is also worth considering whether direct mail could play an impactful role for sales reps, given physicians are likely receiving a high volume of e-mails given the pandemic restrictions on in-person detailing.
Flexible and responsive
While it is impossible to predict exactly when – or if – COVID-19 restrictions will fully ease it is clear that physicians across specialties have been impacted by COVID-19 in multiple, significant ways. Moving forward, it will be important for researchers, pharmaceutical/biotech companies and others who work with those in the health care industry to be flexible and responsive towards physicians’ needs as they navigate this crisis with their patients.
